Have you ever noticed how the first cup of coffee in the morning used to give you a powerful jolt, but now you need two or three just to feel awake? That experience is a perfect everyday example of tolerance. It’s a natural process, but when it involves medications or other substances, it can be a sign of something more serious. Understanding what drug tolerance is is the first step toward recognizing when your body might be sending you an important signal.
If you’re worried that you or a loved one might be developing a tolerance, please know you’re in a safe place. This isn’t about judgment; it’s about giving you clear, compassionate information so you can make the best choices for your health and well-being.
What Is Drug Tolerance?
Drug tolerance occurs when your body adapts to a substance, causing the drug’s effect to diminish over time. As this happens, you need a higher dose to achieve the same effect you once felt with a smaller amount. It’s your body’s way of trying to maintain balance when a substance is used repeatedly. Think of it as your system becoming more efficient at handling the drug, which in turn reduces its impact.
While “drug tolerance” is the clinical term, you might also hear it called “drug resistance” or “desensitization.” It’s important not to confuse tolerance with “drug tolerability.” Tolerability refers to how well you can handle a medication’s side effects. For example, if a prescription makes you feel nauseous, it has low tolerability for you. Tolerance, on the other hand, is about the drug’s primary effect becoming weaker.
Understanding this distinction is crucial because tolerance is a key step in the journey that can lead to dependence and, for some, a substance use disorder. Recognizing it early can make all the difference. For many, this process is a physiological response that can be managed with professional guidance, ensuring both safety and well-being.
Drug Tolerance: Quick Summary
- What it is: A reduced response to a drug after repeated use.
- What it means: You need a higher dose to get the same effect.
- Why it happens: Your body adapts to the presence of the substance.
- Key takeaway: It is a sign to re-evaluate your use with a healthcare professional.
How Does Drug Tolerance Develop?
Developing drug tolerance isn’t a single event but a complex process involving changes in your brain and body. When you repeatedly use a substance, your system works hard to adjust and maintain its natural equilibrium. These adjustments are the mechanisms behind tolerance. Understanding how this happens can demystify the process and highlight why it’s a critical signal to pay attention to.
Let’s break down the main ways tolerance develops, from the microscopic level of your cells to your learned behaviors.
Pharmacological Tolerance (Changes in the Body)
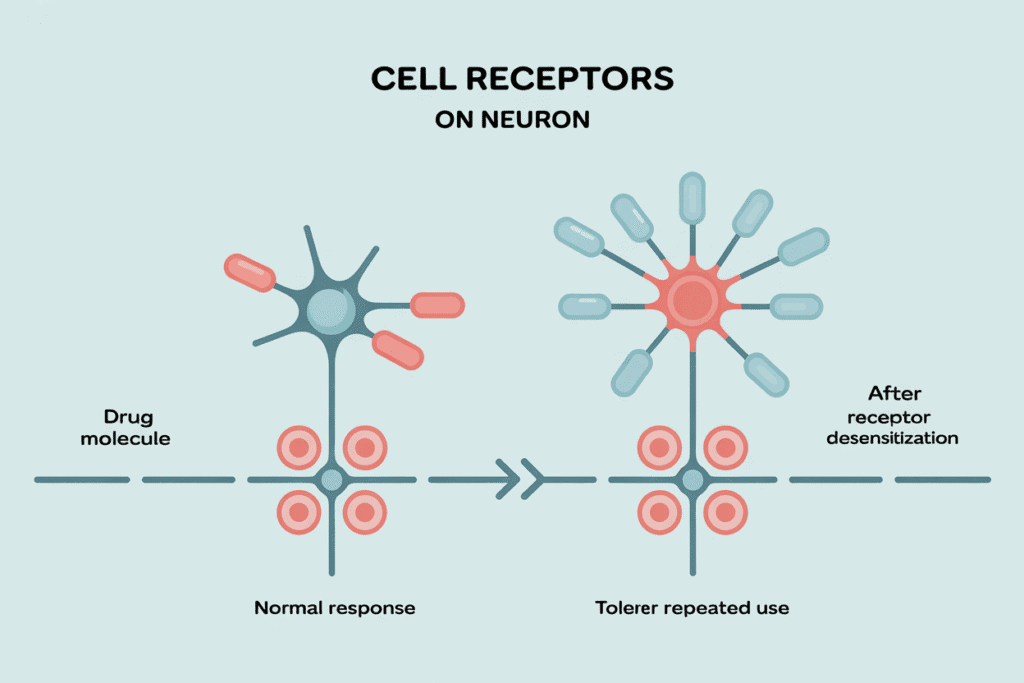
This is where the changes happen at a cellular level, deep within your brain. Your brain cells have receptors that act like docking stations for drug molecules. When a drug is used regularly, these cell receptors can become less sensitive, a process known as receptor desensitization. It’s like the receptors get tired of the constant stimulation and stop responding as strongly. In some cases, the brain may even reduce the number of receptors available. This molecular basis means that more of the drug is needed to activate enough receptors to produce the desired effect. Learning about how drugs affect the brain can provide deeper insight into these powerful changes.
Behavioral Tolerance (Learned Responses)
Behavioral tolerance is about learning to function while under the influence of a substance. It’s a learned adaptation where your mind compensates for the drug’s effect. A common example is when someone who drinks alcohol regularly learns to mask the typical signs of intoxication, like slurred speech or an unsteady gait. Their brain has learned to counteract some of the drug’s impairments, allowing them to appear sober. The environment also plays a role; familiar settings can trigger these learned responses, making the drug’s effect seem weaker than it would in a new situation.
Metabolic Tolerance (Faster Elimination)
Your body, particularly your liver, is designed to break down and eliminate foreign substances. When you use a drug repeatedly, your body can become more efficient at this process. The liver may produce more of the specific enzymes needed to metabolize that substance. As a result, the drug is cleared from your system much faster. This means the same dose won’t last as long or have as much of an impact, leading you to feel you need more of the substance to achieve the same effect.
Tolerance, Dependence, and Addiction: What’s the Difference?
The terms tolerance, dependence, and addiction are often used interchangeably, but they describe different experiences. While they are connected and can happen in sequence, understanding their unique meanings is key. Tolerance is when you need more of a substance to get the same effect. Drug dependence develops when your body adapts to the substance and needs it to function normally. Addiction, now clinically known as a substance use disorder, is a complex brain disease characterized by compulsive drug use despite harmful consequences.
A person can develop tolerance and even dependence on a medication while taking it exactly as prescribed by a doctor, without having an addiction. The key difference lies in the compulsive, often uncontrollable, behaviors associated with addiction. For a clearer understanding of how these concepts differ, our guide on addiction vs. dependence provides more detail.
| Concept | Primary Characteristic | Key Sign | Example |
|---|---|---|---|
| Tolerance | Characteristic: A diminished physical and/or psychological response to a drug | Key Sign: Needing to take a higher dose to achieve the same effect. | Example: After weeks of taking a prescribed pain medication, the original dose no longer provides adequate relief. |
| Dependence | Characteristic: The body adapts to the drug and needs it to function normally. | Key Sign: Experiencing withdrawal symptoms if the drug is stopped or reduced. | Example: Someone who stops their daily coffee habit gets a headache and feels fatigued. |
| Addiction (Substance Use Disorder) | Characteristic: Compulsive drug-seeking and use, despite negative consequences. | Key Sign: Continuing to use the substance despite problems with health, work, or relationships. | Example: Continuing to drink alcohol heavily even after it has caused liver problems and strained family relationships. |
Understanding the Different Types of Drug Tolerance
Drug tolerance isn’t a one-size-fits-all phenomenon. It can show up in different ways, depending on the substance, how often it’s used, and your own unique biology. Getting to know these different types can help you better understand what might be happening in your body and why it’s so important to seek professional advice.
Acute and Chronic Tolerance
Not all tolerance takes weeks or months to develop. Acute tolerance refers to the rapid development of tolerance that can occur after just one or a few doses of a substance. You might notice the effects of a drug are weaker after a few hours than they were when you first took it, even if the amount in your bloodstream is the same. On the other hand, chronic tolerance is the more commonly understood type, which develops over a longer period of repeated use. This is the gradual adaptation that leads someone to increase their dosage over days, weeks, or months.
Cross-Tolerance
Cross-tolerance is a fascinating and important concept where developing tolerance to one drug can cause you to have a tolerance to other drugs in the same class. This happens because many drugs work on the same receptors in the brain. A classic example is with opioids; if you develop a tolerance to oxycodone, you will likely have a tolerance to morphine or heroin as well, since they all act on the same opioid receptors. Similarly, someone with a high tolerance for alcohol may find they need a larger dose of a benzodiazepine to feel its effects. Understanding what happens when drugs are combined is crucial for safety, as cross-tolerance can increase the risk of overdose.
The Dangers of Increasing Drug Tolerance
Recognizing that you’ve developed a tolerance can be unsettling, and it’s natural to feel concerned. It’s a sign that your body has changed in response to a substance, and this change comes with real risks. The biggest danger is that as tolerance grows, you may feel compelled to take increasingly higher doses to get the effect you’re looking for. This can spiral quickly, putting your health and safety at risk.

If this sounds familiar, please know that this is the point where seeking help can change everything. You don’t have to navigate this alone.
Increased Risk of Overdose
There is a direct and dangerous link between tolerance and overdose. As you take a higher dose to overcome tolerance, you move closer to a dose that could be toxic or lethal. Your body’s tolerance to the desired effects of a drug may build faster than its tolerance to the life-threatening effects, like respiratory depression. This risk is especially high if you stop using a substance for a while, causing your tolerance to decrease. If you then return to the previously high dose, your body can no longer handle it, which can easily lead to an accidental overdose.
The Onset of Withdrawal Symptoms
High tolerance is often a strong indicator of physical dependence, meaning your body has adapted to the presence of the drug to function. When the substance is removed or the dose is lowered, you may experience withdrawal symptoms. This withdrawal syndrome is your body’s way of reacting to the absence of the drug it has come to depend on. Symptoms can range from uncomfortable to severe and may include:
- Anxiety, agitation, or irritability
- Nausea, vomiting, or diarrhea
- Muscle aches and pains
- Tremors or shaking
- Insomnia and fatigue
- Sweating and chills
How Is Drug Tolerance Managed?
If you’ve noticed signs of drug tolerance, it’s a clear signal that it’s time to speak with a medical professional. Trying to manage it on your own can be risky, especially if dependence has developed. A doctor can help you understand what’s happening and create a safe, effective plan to address it. Management isn’t about quick fixes; it’s about thoughtful, guided care that prioritizes your long-term health and well-being as part of a comprehensive treatment plan for substance use.
Professional Guidance and Treatment
The first and most important step is to consult a doctor. They can help you create a safe plan to manage tolerance, which might involve adjusting your medication dosage, slowly tapering off the substance to avoid withdrawal symptoms, or switching to a different medication altogether. For many, this is a part of a larger conversation about what addiction treatment entails. Depending on your needs, your doctor might recommend an inpatient or outpatient program. These structured environments are designed to help you manage tolerance, dependence, and withdrawal symptoms safely under medical supervision, while also providing the therapeutic support needed to address the root causes of substance use.
Realizing you’ve developed a drug tolerance is a significant moment of self-awareness. It’s your body’s way of telling you that your relationship with a substance has changed. This isn’t a sign of weakness; it’s a physiological response that carries real risks, from the cycle of dependence and withdrawal to the danger of overdose. But this awareness is also an opportunity,a chance to pause, reflect, and choose a new path forward.
Frequently asked questions
Yes, it’s possible to develop tolerance to nearly any substance you take on a regular basis. This includes prescription medications, over-the-counter drugs, caffeine, and illicit substances. Your body is always working to maintain a stable internal environment, and it can adapt to the presence of many different chemicals.
The speed and degree of tolerance can vary widely. It depends on the specific drug, the dose, how often you use it, and your own unique biology. What might take months for one person could take weeks for another.
No, drug tolerance is typically not permanent. When you stop using a substance or significantly lower the dose, your body can begin to reset its sensitivity over time. This process is often called “resensitization,” and it’s a key reason why seeking professional help is so important.
It’s crucial to understand that a lower tolerance increases the risk of an accidental overdose if you return to using the same high dose you took before. Your body is no longer prepared to handle that amount, which can have dangerous consequences.
Reverse tolerance, also known as drug sensitization, is when a person gets a greater effect from the same dose of a substance that they used to take. It’s the opposite of typical tolerance, where you need more of a drug to feel its effects. You might suddenly feel strong effects from a much smaller amount.
This can sometimes happen with stimulants or with substances like alcohol, especially after long-term heavy use causes damage to an organ like the liver. Because the body can’t metabolize the substance as efficiently, it stays in the system longer, leading to a stronger effect.
There’s no single answer for how long it takes for tolerance to decrease, as it depends on many factors. These include the type of substance used, the dosage, the duration of use, and your individual metabolism and overall health. The timeline is different for everyone.
For some people, tolerance can start to decline within a few days or weeks after stopping use. For others, it may take longer. A doctor can provide the safest guidance on managing this process, especially if dependence and withdrawal symptoms are a concern.
MPower of Exton Is Here to Help
Understanding drug tolerance is the first step, but taking action is what truly matters. Help is available, and you don’t have to navigate this journey alone. If you’re ready to explore your options in a compassionate, judgment-free environment, we are here for you. You can take the first step by calling us at (484) 517-3005 to speak with someone who understands. At MPower Wellness of Exton, we believe in empowering you with the knowledge and support you need to reclaim your health. If you prefer, you can also reach out to us online to start the conversation. Taking this step is a sign of incredible strength.
Sources
National Cancer Institute. (2011, February 2). Definition of drug tolerance. National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/drug-tolerance
National Center for Biotechnology Information. (2003, December 1). The molecular basis of tolerance. PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC3860466/
National Institute on Drug Abuse. (2020, July 6). Treatment and recovery. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
U.S. Government Publishing Office. (n.d.). Behavioral tolerance: Research and treatment implications. U.S. Government Publishing Office. https://www.govinfo.gov/content/pkg/GOVPUB-HE20-PURL-gpo117646/pdf/GOVPUB-HE20-PURL-gpo117646.pdf




